Our recent World Ovarian Cancer Coalition Board of Directors meeting started in the usual way, with a short video from someone with personal experience of ovarian cancer.
Lucía, from Guatemala, is a beautiful, bright, recently married, young mother living with ovarian cancer that has now spread. She spoke clearly and eloquently about not knowing even one other person like herself with the disease, and how this lack of access to a support network outside of her immediate family contributes to a lonely and isolating experience.
In December, Charo, a passionate advocate from ASACO in Spain, told us about the challenge of ensuring women diagnosed with ovarian cancer get access to treatment at specialist centres where there are teams of professionals with specific training and experience dealing with the disease – specialist care that is proven to improve outcomes.
She also shared her anguish about the women she has met who have lost their fertility to ovarian cancer, only to face further heartbreak when denied adoption opportunities because of their cancer history. And at another meeting last year, an ovarian cancer survivor from Nigeria told us about her struggle to get a diagnosis and then to find even basic information about the side-effects of her treatment. She now works with the advocacy group Project PINK BLUE to raise awareness of ovarian cancer and support others who are living with cancer.
We call these personal stories Mission Moments. While members of our Board all have strong personal or professional connections to ovarian cancer, these Moments ground us in our mission and remind us of the urgency of achieving our vision of a world where everyone at risk of, or living with, ovarian cancer has the best chance of survival and best quality of life possible – wherever they may live.
When I saw the recently updated Globocan projections for ovarian cancer, my thoughts immediately turned to the women behind the numbers. Hundreds of thousands of women like Lucía, the women that Charo advocates for in Spain – and the women I meet daily as Chief Executive of Target Ovarian Cancer in the UK. Women who deserve so much better.
These new Globocan figures paint a stark picture of a global escalation of annual ovarian cancer cases and deaths that is even higher than the previous projections. Shockingly, Incidence is set to rise by more than 55% and deaths are forecast to jump by nearly 70% by 2050.
Despite advances in treatment, ovarian cancer remains the most challenging of women’s cancers. Survival rates are low – under 50% in higher income countries – and much lower in less developed countries and regions where sadly the burden of the disease is disproportionately higher.
With no screening test for ovarian cancer, it is often diagnosed at later stages when it is more difficult to treat. Even in countries like the UK, women face significant hurdles. For example, results from a National Ovarian Cancer Audit Feasibility Pilot (OCAFP) show that, in England, approximately 1 in 4 women with advanced stage ovarian cancer do not receive any anti-cancer treatment and only 51% receive both surgery and chemotherapy.
As the only global advocacy organisation focused on ovarian cancer, the World Ovarian Cancer Coalition is committed to making a difference, driving profound and equitable change for all those impacted by the disease through partnerships, evidence, advocacy, and awareness.
Our new 5-year Strategy, From Evidence to Action, sets out a clear roadmap with five strategic goals at its heart. Prevention, access to rapid diagnosis and best treatments, awareness and health literacy and data and evidence, all underpin our call to action to have ovarian cancer recognised as a global health priority and included in global women’s cancer initiatives like the global cervical cancer elimination strategy and the Global Breast Cancer Initiative.
Being Chair of the Board of the of the World Ovarian Cancer Coalition is a huge responsibility but also a great privilege. I believe that the work of the Board, our Coalition, and our 200 advocacy partner organisations remains as relevant as ever, more so in light of these recent projections.
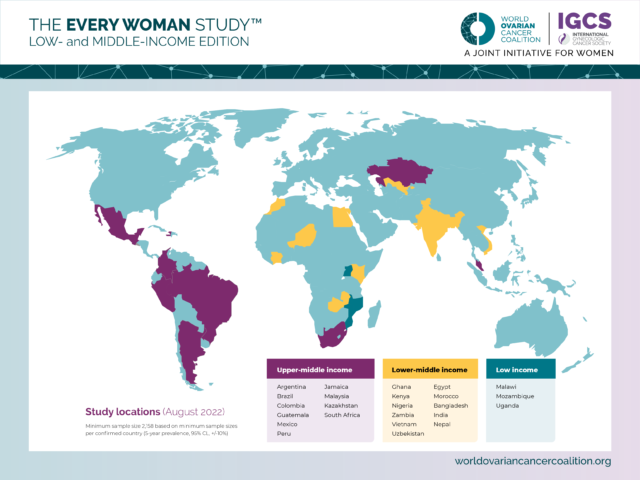
In 2024, the Coalition will be releasing results from our groundbreaking Ovarian Cancer Cost-of-Illness Study and Every Woman Study™: Low- and Middle-Income Edition. Our World Ovarian Cancer Day campaign is entering its 13th year, and we are forging ahead with new partnerships and initiatives to help achieve our vision.
We do not underestimate the challenge we face. But we also know that there are people out there with the experience, vision, and commitment who can help make a difference.
If you think this might be you, l invite you find out more about the Coalition and our plans to recruit up to three members to our Board of Directors so that No Woman is Left Behind.
Annwen Jones OBE
Board Chair, World Ovarian Cancer Coalition
 As organisations and individuals we’ve faced considerable challenges over the past few years. Yet, as we approach the final days of 2023, I find myself deeply thankful for the resilience and commitment shown by my colleagues worldwide. Despite ongoing difficulties such as the escalating cost of living, global conflicts, and the impacts of climate change, our ovarian cancer community remains resolute in ensuring that everyone at risk of, or diagnosed with, ovarian cancer has the best chance of survival and best quality of life possible, no matter where they live.
As organisations and individuals we’ve faced considerable challenges over the past few years. Yet, as we approach the final days of 2023, I find myself deeply thankful for the resilience and commitment shown by my colleagues worldwide. Despite ongoing difficulties such as the escalating cost of living, global conflicts, and the impacts of climate change, our ovarian cancer community remains resolute in ensuring that everyone at risk of, or diagnosed with, ovarian cancer has the best chance of survival and best quality of life possible, no matter where they live. Our own work in this area started with a decision to run a 2SLGBTIQA+/LGBTIQA+ focused awareness campaign during June 2022 under the banner of No Person Left Behind.
Our own work in this area started with a decision to run a 2SLGBTIQA+/LGBTIQA+ focused awareness campaign during June 2022 under the banner of No Person Left Behind. By: Tristan Bilash (he/him/human)
By: Tristan Bilash (he/him/human)